We are closer than ever to being able to 3D print medicines. Here’s why that’s important
3D-printed medicine could be the future of personalised healthcare, with research now suggesting printed tablets have reached a sufficient quality to match the standards set for conventionally manufactured tablets.
Our new study, published in the International Journal of Pharmaceutics, highlights the promise 3D-printed medicines hold for patients.
If we can scale 3D printing to everyday use, the near limitless potential to have medicines customised to your specific health needs may become a reality sooner than you think.
One size doesn’t fit all
For a long time, medicines have been produced with what you might call a “one-size-fits-all” approach, whereby tablets and capsules come in only a set number of doses. But what if those exact doses don’t work for you?
Taking too much or too little of your medication can be hard to avoid when it only comes in set doses. This can have serious consequences when taking important medications such as antidepressants that trigger side effects when the dose is changed too quickly.
The traditional solution to these scenarios has been to try and break the tablet into halves or quarters to get a dose in-between. But this isn’t possible for every tablet, and even if it is, research shows it often ends up with an inaccurate dose.
3D printing can take away the guesswork and provide flexibility for health professionals to truly personalise medicine suited to you.
Read more: Health Check: is it OK to chew or crush your medicine?
Layer by layer
You may have seen 3D printers producing toys, medical devices and even food.
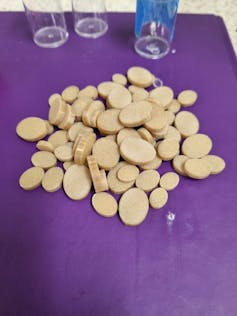
The printing of medicines uses the same technology, building a tablet one layer at a time by melting the medication combined with other approved ingredients to help it dissolve in the stomach. Importantly, the tablet can be 3D printed at any required dose by giving instructions to the machine to print it bigger or smaller.
In our proof of concept study we were able to 3D print tablets containing very accurate doses of caffeine, in a way that would be exceedingly difficult with conventional manufacturing methods.
Rather than choosing a dose based on limited commercial options, we selected the dose first and then designed and printed the tablet accordingly.
While not often thought of as a medicine, the choice of caffeine in this research is important because it is the most widely used behavioural drug worldwide. Trying to cut down on caffeine often causes headaches and nausea because of the challenges in lowering the dose correctly. This is one of many scenarios where a one-size-fits-all approach would fall short.
Compared to attempts to split a conventional caffeine tablet into the same doses, the 3D-printed tablets proved to have far more accurate dosage.
Our results demonstrate a straightforward process for producing “the right medicine for the right patient at the right time”. This is one of the guiding principles of personalised medicine.
Read more: How cancer doctors use personalised medicine to target variations unique to each tumour
A healthcare evolution
Although 3D printing has been around for decades, its use for producing medicines – especially in a hospital or pharmacy environment – is very new.
Australia has rigorous quality control standards for medicines thanks to regulation by the Therapeutic Goods Administration, and it is too early to tell how it will regulate 3D printed medicines.
The United States already has one 3D-printed seizure medication, Spritam, approved by the Food and Drug Administration (FDA). The printing process helps the resulting tablet rapidly disintegrate in the mouth for patients who have trouble swallowing, but does not offer dose customisation.
However, it seems we are on the brink of customised approaches in the clinic, with three new 3D-printed medications receiving FDA investigational new drug approval over 2021-22, and several other clinical trials completed in the last few years.
We envision 3D printers in pharmacies and hospitals for on-site and true personalisation. However, at this stage that doesn’t necessarily mean replacing or even competing with conventional medicines.
The production speed of current 3D printing technologies is much slower than conventional manufacturing. The greatest benefits will likely be for patients with particularly complicated medication regimens, or those taking certain types of medicines like antidepressants. Thus, the people who need it most could have their own tailor-made medicine.
In fact, the possibilities extend further than just choosing the right dose. The practice of pharmaceutical 3D printing could potentially include combining multiple drugs into a single “polypill”, and fully customising features like shape, size, colour, or texture.
We envision an evolution of digital healthcare where 3D printing is combined with technologies like machine learning, artificial intelligence and big data, taking our next big step towards truly personalised medicine.
This future will require a collaborative effort between researchers, health professionals, and regulatory bodies to define the place of 3D printing in healthcare, but could see us picking up our personalised medicine from a local pharmacy or hospital with the touch of a button.

