When COVID-19 or flu viruses kill, they often have an accomplice – bacterial infections
The 1918 influenza pandemic resulted in the loss of over 3% of the world’s population – at least 50 million people. But it wasn’t the flu virus that caused the majority of these deaths.
An analysis of lung samples collected during that flu pandemic indicated that most of the deaths were likely due to bacterial pneumonia, which ran rampant in the absence of antibiotics. Even in more recent history, like the 1957 H2N2 and 2009 H1N1 flu pandemics, nearly 18% of patients with viral pneumonia had additional bacterial infections that increased their risk of death. And the COVID-19 pandemic is no different.
With yet another flu season fast approaching in the midst of the ongoing COVID-19 pandemic, lessening the harm caused by these viruses is important to prevent deaths and reduce infections. However, many deaths associated with the flu and COVID-19 don’t occur at the hand of the virus alone. Instead, it’s a secondary bacterial infection that is often at the root of the devastating consequences attributed to an initial viral infection.
I am an immunologist who studies why and how cells die during bacterial and viral infections. Understanding the synergy between these microbes is critical not only for effective diagnosis and treatment, but also for managing current pandemics and preventing future ones. My colleagues and I published a study showing how an immune system protein crucial to fighting against viruses also plays an indispensable role in fighting bacteria.
Viruses and bacteria team up
Multiple pathogens can cause multiple infections in different ways. Scientists distinguish each type based on the timing of when each infection occurs. Coinfection refers to two or more different pathogens causing infections at the same time. Secondary or superinfections, on the other hand, refer to sequential infections that occur after an initial infection. They’re often caused by pathogens resistant to antibiotics used to treat the primary infection.
How viral and bacterial infections interact with each other increases the potential harm they can cause. Viral respiratory infections can increase the likelihood of bacterial infections and lead to worse disease. The reason why this happens is often multifaceted.
Within your respiratory tract, the epithelial cells lining your airways and lungs serve as the first line of defense against inhaled pathogens and debris. However, viruses can kill these cells and disrupt this protective barrier, allowing inhaled bacteria to invade. They can also change the surface of epithelial cells to make them easier for bacteria to attach to.
Viruses can also alter the surface of epithelial and immune cells by reducing the number of receptors that help these cells recognize and mount a response against pathogens. This reduction means fewer immune cells report to the viral infection site, giving bacteria an opening to launch another infection.
Influenza, COVID-19 and bacterial infections
Patients who have a bacterial infection at the same time they’re battling the seasonal flu are more likely to wind up in a hospital. Nearly a quarter of patients admitted to the ICU with severe influenza also have a bacterial infection. One study on the 2010 to 2018 flu seasons found that nearly 20% of patients admitted to the hospital with flu-associated pneumonia had acquired bacterial infections.
Another study of patients hospitalized with viral or bacterial infections found that nearly half had a coinfection with another pathogen. These patients also had nearly double the risk of dying within 30 days compared to those with only a single infection.
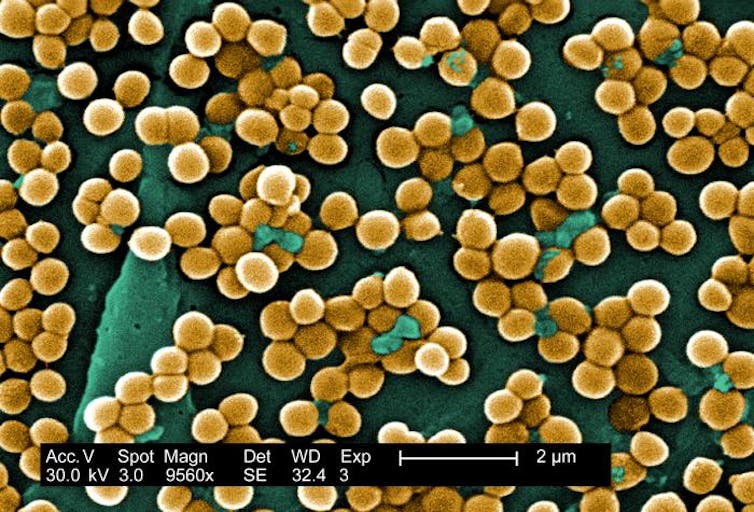
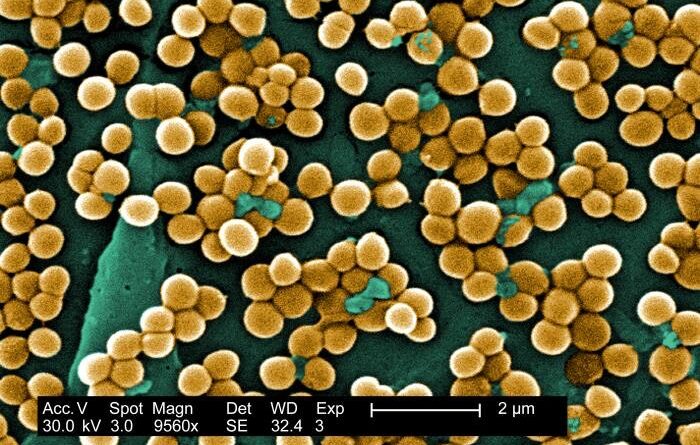
Interestingly, the two bacteria species most commonly involved in coinfections with the influenza virus are Streptococcus pneumoniae and Staphylococcus aureus, which normally exist in the respiratory tract without causing disease. However, the influenza virus can damage the cell barrier of the lungs and disrupt immune function enough to make patients susceptible to infection by these otherwise benign bacteria.
Secondary bacterial infections are also exacerbating the COVID-19 pandemic. A 2021 review estimated that 16% to 28% of adults hospitalized for COVID-19 also had a bacterial infection. These patients stayed in the hospital for twice as long, were four times more likely to need mechanical ventilation and had three times greater odds of dying compared to patients with only COVID-19.
Addressing secondary and coinfections
The immune system responds differently to viruses and bacteria. Antivirals don’t work on bacteria, and antibiotics don’t work on viruses. A better understanding of what pathways the body uses to regulate both antiviral and antibacterial infections is critical to addressing secondary and coinfections.
Recent work by my colleagues and me may provide a clue. We sequenced the RNA of one type of immune cell, macrophages, in mice to identify what molecules were present in cells that were either protected from or died due to bacterial infection.
We identified Z-DNA binding protein (ZBP1), a molecule already known to play a regulatory role in how the immune system responds to influenza. Specifically, ZBP1 detects influenza viruses within the lungs and signals infected epithelial and immune cells to self-destruct. This induced cell death eliminates the virus and promotes recruitment of additional immune cells to the infection site.
Building off this finding that ZBP1 is important for fighting viral infection, we found that macrophages infected with Yersinia pseudotuberculosis, a type of bacteria that causes foodborne illness, also use this protein to initiate cell death. This limits bacterial replication while also sending inflammatory signals that help clear bacteria.
These findings raise the possibility that ZBP1 may play a dual role in how the body responds to viral and bacterial infections. It’s possible that treatments that increase ZBP1 in certain types of cells may be useful in managing bacterial and viral coinfections.